The Why
Vision is a precious sense, integral to our daily lives and overall well-being. Regular eye exams by a qualified optometrist are essential for maintaining good vision and detecting potential eye conditions early. Despite the importance of eye health, many people overlook the need for regular eye care.
#1 Early Detection of Eye Conditions:
One of the primary reasons to see an optometrist regularly is to detect and manage eye conditions early. Many eye diseases, such as glaucoma, macular degeneration, and diabetic retinopathy, develop gradually and may not present noticeable symptoms in the early stages. A comprehensive eye exam can detect these conditions before they cause significant vision loss, allowing for timely intervention and treatment.
#2 Rx Updates:
If you wear glasses or contact lenses, regular visits to the optometrist are essential to ensure that your prescription is up to date. Vision changes can occur gradually over time, and an outdated prescription can lead to eyestrain, headaches, and difficulty seeing clearly. By visiting an optometrist regularly, you can ensure that your corrective lenses are providing you with the best possible vision.
#3 Monitoring Eye Health:
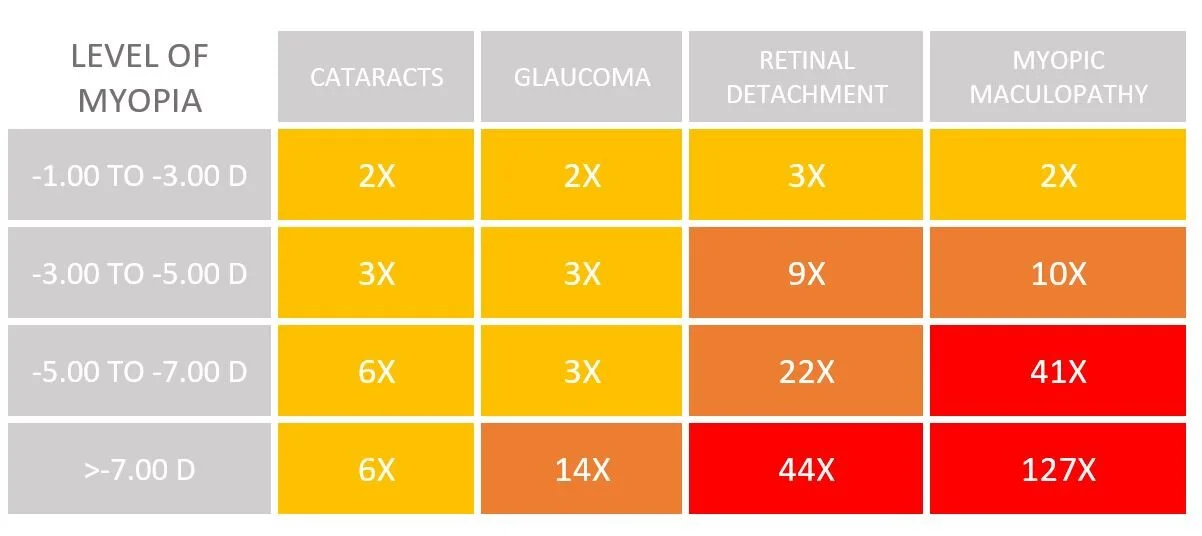
In addition to checking your vision, optometrists also examine the overall health of your eyes. They can identify signs of eye conditions such as cataracts, retinal detachment, and dry eye syndrome. By monitoring your eye health regularly, optometrists can provide early treatment and management strategies to preserve your vision and prevent complications.
#5 Detecting Systemic Health Conditions:
Believe it or not, your eyes can provide valuable insights into your overall health. During an eye exam, optometrists can detect signs of systemic conditions such as diabetes, hypertension, and high cholesterol. These conditions can affect the blood vessels in the eyes, leading to changes that are visible during an exam. Early detection of these conditions can lead to timely referral to a primary care physician for further evaluation and management. Your eye doctor will put dilation drops into your eyes so they could do a 3D scan to better assess your retina, optic nerve connection, and vasculature.
#6 Children's Eye Health:
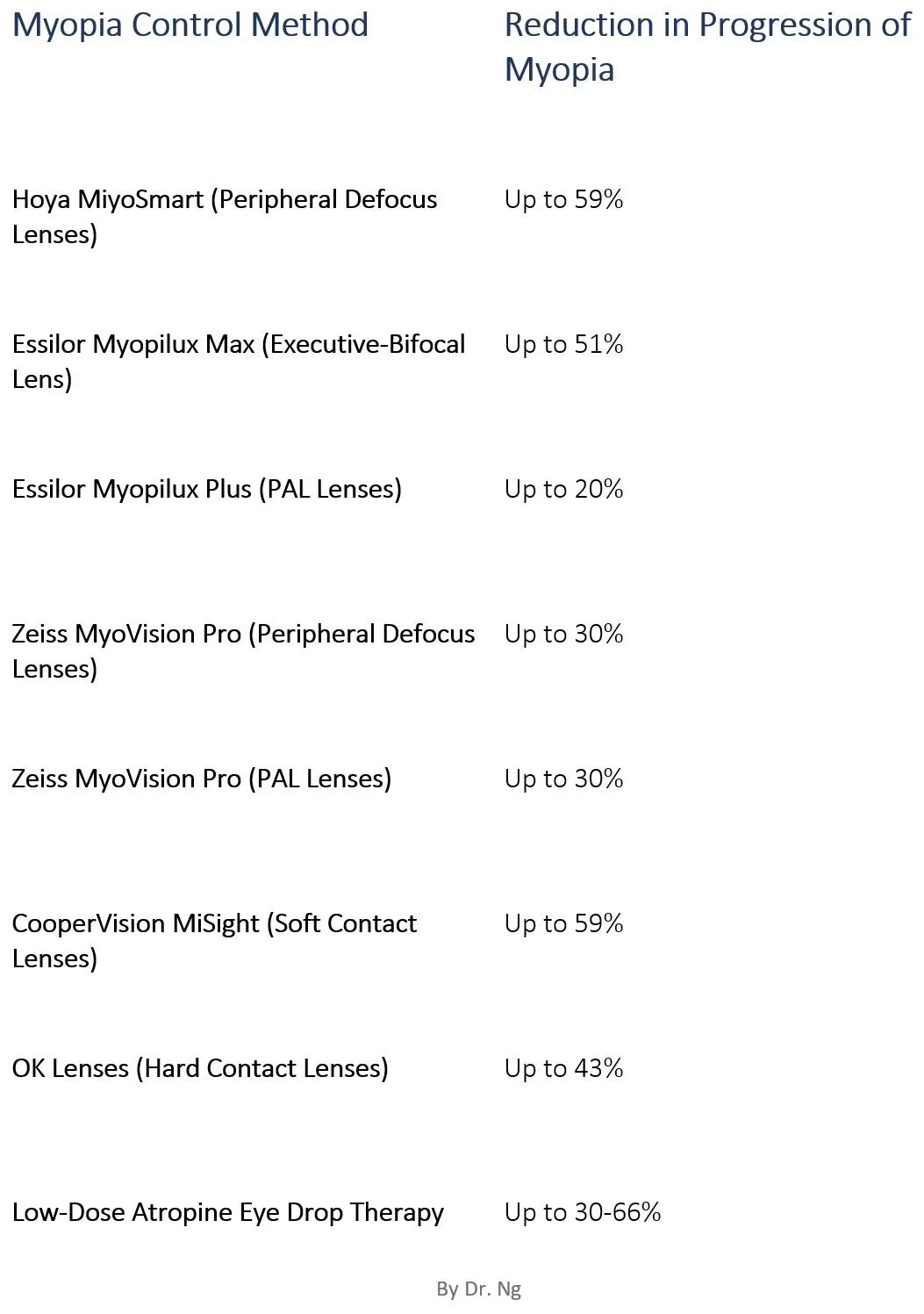
Children's eye health is particularly important, as vision problems can affect their learning and development. 80% of our learning is through vision. Regular eye exams can detect issues such as refractive errors, lazy eye (amblyopia), and eye alignment problems (strabismus) early, when they are more easily treated. Early intervention can prevent vision problems from impacting a child's academic performance and quality of life. Myopia control therapy is a new form of treating myopia by preventing the eye from getting worse through therapeutic glasses, contacts, night lenses and eye drops.
schedule an eye exam today
Seeing an optometrist regularly is crucial for maintaining good eye health and overall well-being. From early detection of eye conditions to ensuring that your corrective lenses are up to date, optometrists play a vital role in preserving your vision and quality of life. Don't neglect your eye health—schedule a comprehensive eye exam with an optometrist today. Your vision deserves professional care.